Key UC Contact
What We Did
I’m developing an implantable, wireless sensor system to monitor the progress of bone fracture healing and spinal fusion. This is a patented design which requires no batteries, as it uses electromagnetic waves to both power the device and transmit the data through the tissue.
The purpose of my research is to improve patient outcomes after orthopaedic surgery by incorporating a “smart” implant that will allow clinicians to determine when bone healing or spinal fusion has occurred. Interrogation of the smart implant will be able to be done by a general practitioner, enabling specialist interpretation and care at a distance.
My work will represent a paradigm shift in orthopaedic diagnostics by a) reducing patient disability period, b) providing actionable data on when an implant can be removed, and c) determining when a patient can return to employment or normal activities.
The sensor is precise enough to differentiate between unfused, early fusion, and fused bone states, whilst being appropriate for use in a clinical environment. The technology uses the same titanium materials currently used in pacemakers (e.g. reliable moisture protection for the sensor) and orthopaedic fixations (equivalent biocompatibility to existing bone fixations). Wireless power and communication are provided via technology developed by my colleagues at the Auckland Bioengineering Institute (ABI), and we are conducting a 6-month pilot sheep study in 3 animals later this year at Lincoln University. I recently won both the ChristchurchNZ HealthTech Supernode Challenge and the MedTech/CMDT HealthTech Award for Best Translational Research Project. I am now seeking funding to commercialise this technology.
Who Was Involved
UC Research & Innovation (Rebecca Warr, Hamish McGowan, Elizabeth Hopkins), UC Nanofabrication Lab in EE (Maan Alkaisi, Volker Nock), UC Postgrads and students (Simon Blue, Seb Jones, Cameron Woods, Micaela Cooper, George Howat).
University of Auckland Bioengineering Institute (David Budgett, Daniel McCormick), and Masters’ students (Negar Zoka, Angus Malcolm). Also, orthopaedic surgeon Dr Paul Monk, and Lincoln University’s Nadia Mitchell and Martin Wellby.
Veterinary orthopaedic surgeon (Dr Brent Higgins), Callaghan Innovation Advanced Materials Group (Karl Dahm), MedTech CoRE and KiwiNet seed funding.
Why It Matters
There has been a huge increase in implanted medical devices, and yet our ability to detect when bone has healed, when an implant needs to be removed, or when an implant has failed remains virtually unchanged. The use of wireless, implantable sensors changes that, providing current information about the state of the implant that is accessible to a clinician even when patients are in remote locations.
Learn More
- Munro DS., Tsai EC., Lingley AR. and Khbeis MT. (2016) Development of a Microfabricated Sensor System to Measure Lumbar Spinal Fusion. In 3(Biomedical and Biotechnology Engineering): 7. ASME Digital Collections. http://dx.doi.org/10.1115/IMECE2016-65703
- Deborah’s research profile: https://researchprofile.canterbury.ac.nz/Researcher.aspx?Researcherid=5240192
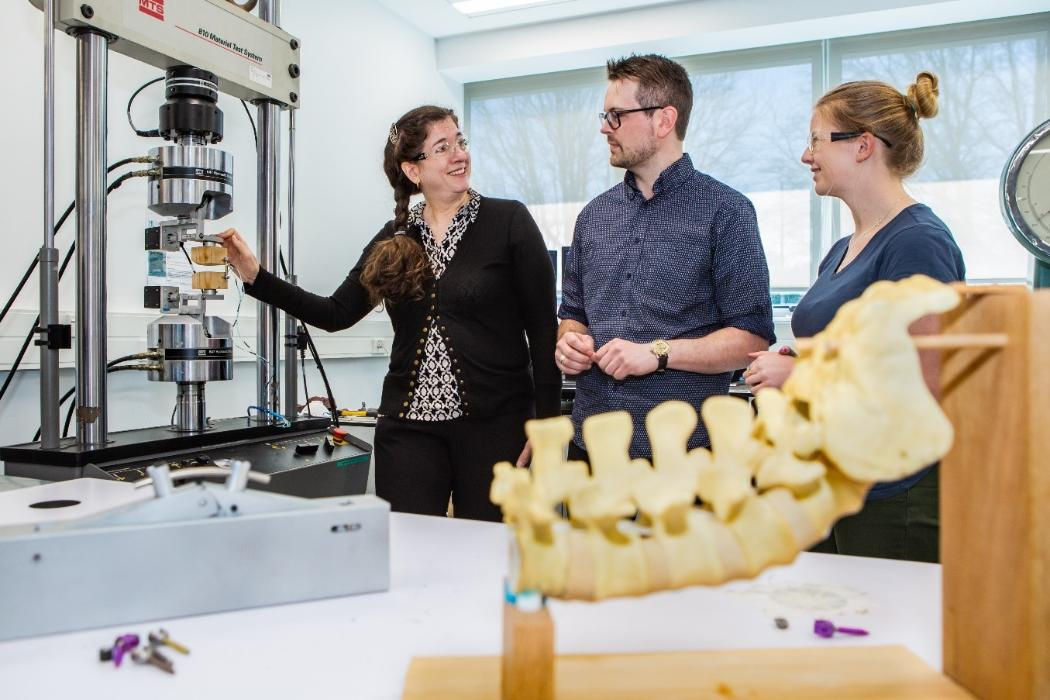
Photo Caption:
Debbie Munro demonstrates biomechanical testing of sensor system to Simon Blue and Katie Ellis